Take a deep breath. And take a moment to appreciate the amazing physiology of your lungs at work.
Most of us take for granted that the air we breathe is diffused across 500 million tiny balloon-shaped air sacs in our lungs called alveoli. Each is just the diameter of a single human hair, but collectively they make up a surface area half the size of a volleyball court. Across that vast network, each alveolus is surrounded by capillaries, carrying oxygen into and carbon dioxide out of your bloodstream.
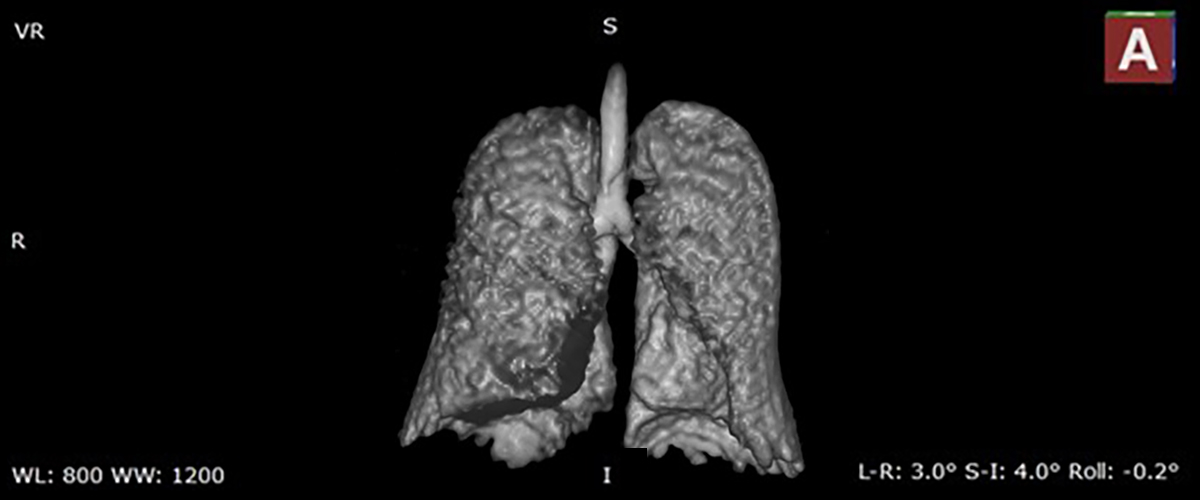
Now, MagLab researchers and doctors at the University of Florida are testing a new MRI technique that can deliver images of that complex process as never seen before. The technique, set for clinical trials at the MagLab's MRI facility at UF, has the potential to revolutionize lung imaging and improve treatment of diseases such as asthma and COPD.
"It's incredibly powerful technology" according to Dr. Borna Mehrad, the chief of pulmonary care at UF Health and a pulmonary disease researcher.
The new technique combines hyperpolarized xenon gas and magnetic resonance imaging (MRI) to yield highly detailed MRI images of lung function. At the MagLab's Advanced Magnetic Resonance Imaging and Spectroscopy (AMRIS) Facility at UF, researchers have just conducted their first test of xenon MRI.
The technology is able to show doctors the gas inside an alveolus, gas dissolved in the lung that has not yet crossed into the bloodstream, and gas that’s just passed into the blood stream, associated with hemoglobin. Each can be measured separately, providing important in-depth data.
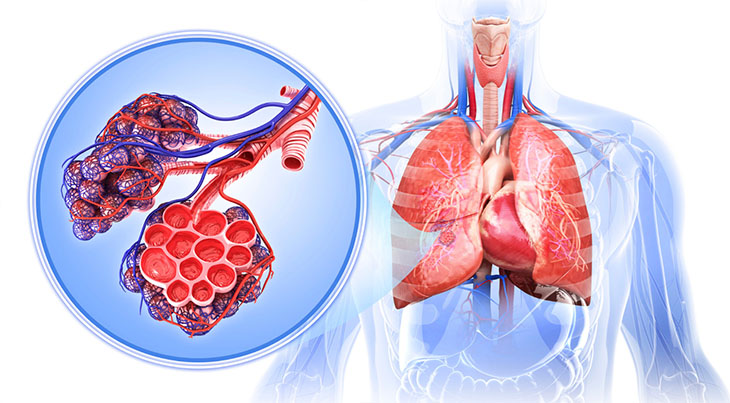
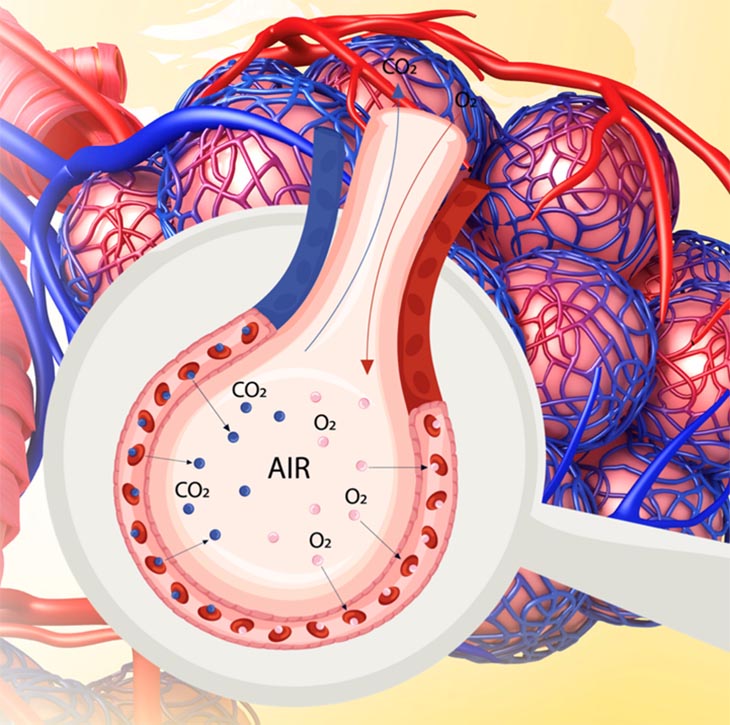
Illustrations of the lungs and alveoli, and how oxygen and carbon dioxide are exchanged with the bloodstream within each alveolus.
"You can see where alveoli are ventilated, which are partially ventilated, which are not ventilated," Dr. Mehrad explained, "This technology has the potential to really expand our ability to assess lung disease."
Getting a good look at the lungs has long been a challenge. Currently, doctors analyze lung function using technology developed in the 1950's called a pulmonary function test, or PFT. PFT has patients take a deep breath and blow into a machine, providing only a measure of overall lung function. Doctors cannot zero in on which areas of the lung may be impaired and which may be functioning normally. Other technologies, X-rays and CT scans, offer only a snapshot of lung structure, but not function. Traditional MRI, which relies on hydrogen protons in water, is also ineffective in assessing the lungs.
"Lungs are filled with air," said Jens Rosenberg, AMRIS Facilities Manager of Clinical MRI Instrumentation who helped test the new technique. "Air is usually a big problem. There's not really anything we can look at," said Rosenberg.
That's where the xenon comes in. The inert, noble gas is harmless and doesn't react with anything in the lungs.
"However, if you just inhale regular xenon we can't get a detailed image," Rosenberg explained.
A hyperpolarization process uses the metallic chemical rubidium and lasers to create what Rosenberg calls a "quantum dance to put xenon into a higher energy state." That amplifies the MRI signal seven to eight times to generate a clear picture. The hyperpolarizing system is on loan to MagLab's advanced MRI team from Polarean, a medical technology company working to commercialize the system.
Xenon MRI patients wear a special vest containing a radiofrequency coil that detects the xenon signal. They inhale the hyperpolarized gas and hold their breath for about 15 seconds while the MRI scans their lungs. Patients may have a high-pitched voice for a few minutes, like when you inhale helium, and a brief light-headed feeling, but ultimately end up with lung images with much greater detail than is available with other methods.
Dr. Mehrad cautions that scientists are still in the early stages of defining xenon MRI’s capabilities, but notes that the imaging holds promise for treatment of asthma, chronic obstructive pulmonary disease (COPD), cystic fibrosis, pulmonary hypertension, sarcoidosis and many other lung diseases.
Mehrad points specifically to this technique's potential for transforming asthma treatment. Doctors often struggle to identify which patients will respond to which asthma treatments, but xenon MRI’s detailed images may help them pinpoint which treatment works best.
"What we want to do is study it in a variety of lung diseases and see if you can identify subsets of patients who would benefit from a treatment," Mehrad said.
By the end of the year, researchers will start a clinical trial using the new imaging on patients from UF Health's pulmonary clinic.
"Now that we have done the first image, we are excited to continue," said Rosenberg.
Story by Edan Schultz